The goal of the cardiac catheterization rotation is to train fellows in the diagnostic and therapeutic role of cardiac catheterization in the management of all types of cardiovascular disease including coronary, structural, primary myocardial, pericardial, congenital, and peripheral vascular disease.
Fellows will also be expected to attend a weekly cardiac catheterization conference designed to address the role of cardiac catheterization/intervention in various disease processes. Fellows will also be expected to interact professionally with patients, families, and all members of the invasive cardiology team.
The goals and objectives of training in the invasive laboratory include:
- Hemodynamic assessment – recording of pressures in the cardiac chambers and the vascular tree.
- Determination of cardiac function, evaluation of shunts, and valvular disease.
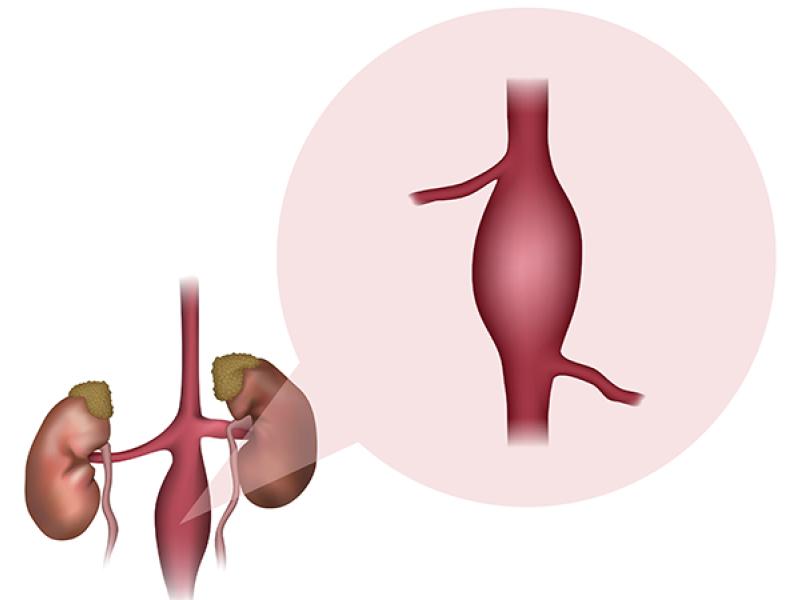
- Angiography to evaluate the presence of vascular obstruction or other abnormalities, contractile function the left ventricle, and valvular lesions.
- Therapeutic procedures such as pericardiocentesis, intra-aortic balloon pumping, endomyocardial biopsies, and temporary transvenous pacemaker insertion.
Rotation leaders
- Dr. Arun Kumar (MUHC)
- Dr. Kul Aggarwal (VA)
Objectives
1st year fellow (one rotation)
- Know indications and contraindications for right and left heart catheterization as well as associated complications.
- Explain the procedure, potential complications, risks/benefits/alternatives to patients and families and obtain informed consent.
- Recognize comorbidities that lead to increased risk and the appropriate interventions to mitigate risk (including kidney disease).
- Understand fundamentals of radiation safety.
- Understand mechanism of action of anesthetic, antiplatelet, anticoagulant, and vasoactive medications.
- Perform intravascular catheter insertion to obtain both arterial and venous access (with ultrasound when indicated) and obtain hemostasis.
- Recognize coronary anatomy, variations, congenital abnormalities, and coronary blood flow physiology.
- Perform coronary angiography and catheter manipulation under supervision.
- Interpret coronary angiography with assistance.
- Perform right heart catheterization under supervision.
- Review fundamentals of hemodynamics in patients with valvular disease and heart failure.
- Perform left ventriculography under supervision and determine left ventricular ejection fraction.
- Manage complications of cardiac catheterization.
- Understand peripheral vascular anatomy.
- Understand indications, contraindications, and complications of peripheral vascular angiography.
- Review indications and potential complications of pericardiocentesis.
- Review indications and potential complications of endomyocardial biopsy.
2nd year fellow (two to four rotations)
In addition to the above:
- Review fundamentals of hemodynamics in patients with myocardial, pericardial, and pulmonary vascular diseases.
- Integrate findings of coronary angiography, ventriculography, and hemodynamic assessments to formulate appropriate management plan in the context of the clinical scenario.
- Review indications for percutaneous coronary intervention.
- Recite indications for vascular closure devices and associated complications.
- Assist in procedures of unstable and complex patients, including those with acute coronary syndromes, complex valvular heart disease, and congenital heart disease.
- Interpret coronary angiography, graft angiography, ventriculography, and right heart catheterization hemodynamic data independently.
- Complete COCATS level 1 training which includes participation in at least 100 diagnostic cardiac catheterization procedures. Of these, at least 50 should involve coronary angiography and at least 25 should involve hemodynamic assessment of valvular, myocardial, pericardial, or congenital heart disease.
3rd year fellow (two to three rotations)
In addition to the above:
- Perform diagnostic coronary angiography, ventriculography, and left and right heart catheterization independently.
- Place intra-aortic balloon pump in emergent situations.
- Perform pericardiocentesis.
- Perform transvenous pacemaker insertion.
- Assist in percutaneous coronary interventions.
- Complete COCATS level 2 training, if applicable to fellow’s career path, to include performance of at least 300 diagnostic cardiac catheterization procedures.
Fellow responsibilities
- During cardiac catheterization rotations the fellow is expected to be present in the catheterization laboratory for the entire workday (7:00 am – 5 pm), unless assigned to clinic or attending mandatory fellow conferences, and report to the Charge Person in the cath lab regarding the case assignment.
- The fellows are expected to place pre-procedure orders for outpatient procedures the day prior to scheduled procedures, know the patients and perform a relevant cardiovascular physical exam on day of admission, including their vascular access sites prior to the admission of the patient to the laboratory, obtain consent, perform a pre-sedation evaluation, and document findings in electronic medical records.
- Post procedure, fellows are expected to place admission/discharge orders and sign out to the team on call that night regarding patients who are staying on observation/short stay. In AM, fellows are expected to assess and discharge patients who stay overnight.
- The fellows will master the catheterization skills progressively over the course of 3 years and are expected to perform several diagnostic catheterizations with the attending present but not scrubbed during their last rotation.
- Fellows will interpret studies, generate a report in conjunction with the attending physician, and arrange appropriate follow-up.
- Fellows will generate a discharge summary for outpatients undergoing catheterization studies.
- Participate in emergency procedures when assigned as the "on call" fellow.
The fellow will be able to meet minimum performance and interpretation guidelines based on their year of training. In general:
First Year Fellow
- Learning vascular access
- Achieving hemostasis, sheath removal
- Setting up pressure manifolds or Acist device
- Learning basic hand washing techniques, gowning and gloving
- Maintaining sterility in cardiac catheterization lab
- Performing diagnostic coronary angiography and left ventriculography
- Performing and interpreting right heart catheterization
- Understanding basics of interventional cardiology especially indications for interventional procedures and selection of patients for surgical referral
- Hemodynamics and valve area calculations
- Assessment of severity of lesion stenosis
- Interpretation of coronary and peripheral angiograms
Second and Third Year Fellows
In addition to skills acquired at the previous level
- Assisting in percutaneous transluminal coronary angioplasties
- Assisting in intra-coronary stent placements
- Insertion of temporary transvenous pacemaker
- Insertion and care of intra-aortic balloon counterpulsation devices
- Take calls for emergent cardiac catheterization laboratory procedures
- Assisting in other interventional procedures such as rotablations, directional coronary atherectomies, laser angioplasties, and thrombectomy
- Assisting in balloon valvuloplasties
- Learning techniques of lesion assessments including “setting up” angiographic views, analyzing lesions with quantitative coronary angiography
- Planning interventional strategies
- Assisting in intra-coronary doppler flow studies and pressure wire measurements
- Assisting in the performance and interpretation of intravascular and intracardiac ultrasound studies
- Assisting in the performance of PFO and ASD closures
Attending responsibilities
- Directly supervise all procedures.
- Provide immediate and post-procedure feedback to the fellow.
- Assign progressive responsibility for the procedure based on performance milestones achieved.