Post-graduate physician training, known as residency, develops skills and expertise within a medical specialty. During five to seven years of surgical training, medical school professors determine the level of clinical competency, confidence and decision-making skills of each resident physician through personal observations. However, a recent study at the University of Missouri School of Medicine has shown that levels of perspiration can provide an objective evaluation of the surgical skills of resident physicians.
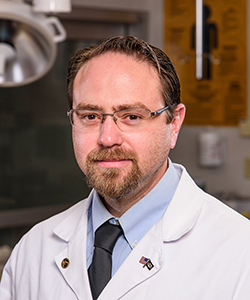
“Within surgical education, skill evaluation is based on a subjective assessment, which essentially is a gut feeling,” said Jacob Quick, MD, assistant professor of acute care surgery at the MU School of Medicine and lead author of the study. “There is a need for an objective, impartial way to determine surgical ability and a resident’s capacity to operate independently. We monitored electrodermal activity during actual surgical procedures. We hypothesized that as training progressed, resident responses to the stress of performing surgical procedures would decline in relationship to their experience level.”
Electrodermal activity, or EDA, is a method of measuring electrical characteristics of the skin. The amount of electrical activity conducted across skin is related to psychological or physiological stimulation. As this increases, glands controlled by the sympathetic nervous system are activated and produce sweat. Because water is a good conductor of electrical activity, sweat can be used to measure emotional and sympathetic responses to stress.
“Essentially, the more nervous we are, the more we sweat,” said Quick, who also serves as a trauma surgeon at MU Health Care. “The more we sweat, the more electrical activity is conducted across the skin. We used skin response sensors worn by residents to monitor their EDA while they performed laparoscopic gallbladder surgeries.”
Fourteen general surgery residents and five faculty physicians participated in the study over an eight-month period. EDA responses were measured during each of the 130 surgical procedures monitored. The results were compared to determine common points during procedures where surgeons experienced different levels of EDA responses.
“Our initial findings indicated that at crucial points during the procedures, residents’ EDA increased as much as 20 times more than experienced faculty performing the same surgery,” Quick said. “However, over the course of the study, and as their proficiency developed, surgical residents’ EDA levels began to lower in accordance with their experience.”
Quick said that although the next step will be to add stop-action photography into the evaluation process to further explore objective assessments, EDA may not become a standard training option any time soon.
“This type of monitoring is relatively easy to accomplish,” Quick said. “It can be cost prohibitive, though. While the sensors are reusable, initial equipment costs can be as much as $10,000. Additionally, our study was limited to 14 resident physicians at a single medical center. However, this objective measure of surgical ability could have far-reaching implications on surgical education in the future.”
The study, “Objective Measurement of Clinical Competency in Surgical Education,” recently was published in the Journal of Surgical Education. Research reported in this publication was supported by the Association of Program Directors in Surgery and the Association for Surgical Education. The researchers have no conflicts of interest to declare related to this study.