Small study shows promise in improving sleep but more research needed.
Insomnia is the most common sleep disorder in children with autism spectrum disorder (ASD) and affects up to 80% of children with ASD. Several studies report a strong link between insomnia and the severity of ASD-related symptoms, including social impairment, communication difficulties and anxiety. Insomnia’s impact on children with ASD can affect the entire family, causing sleep loss and additional stress for parents. Now, researchers from the University of Missouri School of Medicine and the MU Thompson Center for Autism and Neurodevelopment have found cognitive behavioral therapy can improve child and parent sleep, child behavior and parent fatigue.

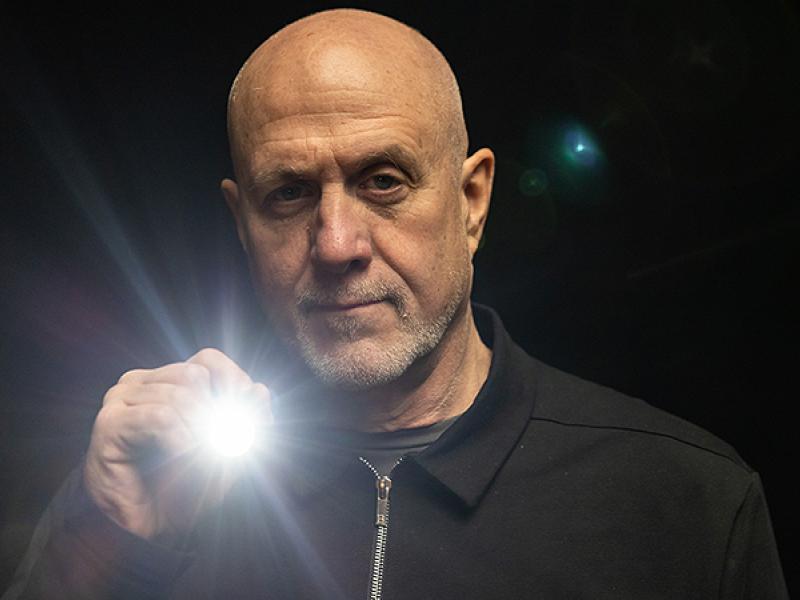
“You can’t make yourself sleep better,” said Christina McCrae, PhD, professor in the Department of Psychiatry at the MU School of Medicine. “Sleep is a natural process. It’s not an intentional activity. The first step to curing insomnia for children with ASD involves setting the stage for the circadian clock and the sleep rhythm to work the way they are meant to work.”
McCrae’s study involved 17 children ages 6 to 12 with ASD who were also diagnosed with insomnia. Seventeen parents of the children also participated in the study. Both parents and children completed daily electronic sleep diaries which detailed how long it took to fall asleep, total sleep time and other factors. They also wore electronic devices on their wrists to measure limb movement, which is an objective way to measure sleep quality. Each family completed eight, 50-minute cognitive behavioral therapy sessions with therapists designed to address the barriers preventing sleep.
“Instead of a uniform plan for all participants, we targeted each family’s most pressing concerns and organized our therapy modules to address those key issues in the first few sessions,” McCrae said. “That provided more time in later sessions for families to refine their techniques with help from their therapist.”
Following the eight sessions of therapy, data collected from the devices and diaries showed the children who participated showed sleep and behavior improvements. After one month, 85% no longer experienced insomnia. Parents involved in the study experienced less fatigue and better sleep, according to the monitors and self-reporting diaries.
“We looked at how many sessions the families attended, how well the families understood the treatment, and the subjective and objective outcomes,” McCrae said. “As the paper shows, the outcomes are amazing. While it makes sense that child sleep impacts parental sleep, I didn’t expect the parents to see as much improvement as they did in the study.”
McCrae hopes to expand this pilot study into a randomized controlled trial with an active control group and a more diverse sample. She also plans to introduce a telehealth version of the cognitive behavioral therapy to assist families in rural areas or those unable to travel.
In addition to McCrae, the study authors include University of Missouri colleagues Ashley Curtis, PhD, post-doctoral fellow, Department of Psychiatry; Pradeep Sahota, MD, associate professor and chair of neurology at the MU School of Medicine; Chelsea Deroche, PhD, assistant professor of biostatics and research design, MU School of Medicine; Melissa Munoz, doctoral student; Dillon McCann and Kevin McGovney, undergraduate assistants, Mizzou Sleep Research Lab; Julie Muckerman, research specialist, and Nicole Takahashi, research core administrator, Thompson Center for Autism and Neurodevelopmental Disorders. Other co-authors represented the University of Virginia; Children’s Hospital in Aurora, Colorado; and the University of Hong Kong.
The study, “Cognitive Behavioral Treatment of Insomnia in School-Aged Children with Autism Spectrum Disorder: A Pilot Feasibility Study,” was recently published in the journal International Society for Autism Research. Research reported in this publication was supported by a University of Missouri Research Board award. The authors of the study declare that they have no conflicts of interest related to this study. The content is solely the responsibility of the authors and does not necessarily represent the views of the funding agencies.