Scoliosis is the most common spinal deformity affecting pediatric patients. A posterior spinal fusion (PSF) is the gold standard treatment for patients with curves exceeding 45 degrees, but the procedure’s drawbacks include the loss of spinal mobility, persistent pain and adjacent segment disc disease. However, a new retrospective study from the University of Missouri School of Medicine and MU Health Care shows an alternative to PSF called vertebral body tethering (VBT) yields promising results with fewer long-term consequences for a specific group of scoliosis patients.
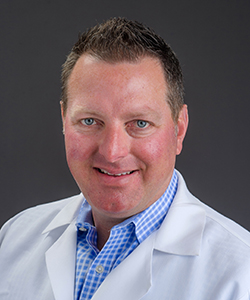
VBT is an alternative to PSF for scoliosis patients who still have growth remaining and flexibility of their spine. Screws are attached in a minimally invasive fashion to the thoracic or lumbar vertebra in the curved area of the spine. A polyethylene cord connects the screws and tension straightens the spine, correcting the scoliosis. MU Health Care is one of only a handful of medical centers in the U.S. offering the procedure. Pediatric orthopaedic surgeon Dan Hoernschemeyer, MD, is the principal investigator for the study and has performed more than 85 VBT surgeries on patients from around the country.
“If the child’s spine has more than 45 degrees of scoliosis and still has some growth remaining, VBT is a way to correct the scoliosis, preserve motion and modulate normal growth instead of fusing it,” Hoernschemeyer said. “Our study examined the radiographic and clinical outcomes of idiopathic scoliosis patients with various curve patterns treated with VBT.”
Hoernschemeyer and his team conducted a retrospective review of 29 consecutive patients with 2-5 year follow-ups. Successful outcomes were defined by a curve of less than 30 degrees in patients who reached skeletally maturity and had not receive a PSF. At the latest follow-up, 27 patients reached skeletal maturity and 74% achieved clinical success.
“Despite our patient population being slightly more mature at the time of surgery than when compared to previous studies, we found a higher success rate and a lower revision rate,” Hoernschemeyer said. “Our overall revision rate was 21% and a PSF was avoided in 93% of patients, indicating that VBT may be a reliable treatment option for adolescent scoliosis.”
The most common complication that led to revision involved tether breakage. Fourteen patients experienced a broken tether, and half required either a revision surgery or PSF.
“While the exact role of VBT in the management of adolescent scoliosis continues to be defined, the data from this study supports the fact that this surgical procedure should be considered as a treatment option for children with scoliosis and an alternative to fusion,” Hoernschemeyer said.
In addition to Hoernschemeyer, the study authors include MU colleagues Melanie Boeyer, PhD, post-doctoral fellow in the Department of Orthopaedic Surgery; Nicole Tweedy, DNP-PNP, pediatric nurse practitioner; Sumit Gupta, MD, associate professor of orthopaedic surgery; Dana Duren, PhD, director of orthopaedic research; and Venkataraman Ramachandran, MD, associate professor of clinical surgery and child health.
Hoernschemeyer’s study, “Anterior Vertebral Body Tethering for Adolescent Scoliosis with Growth Remaining: A Retrospective Review of Two to Five Year Postoperative Results,” was recently published in the Journal of Bone and Joint Surgery. The authors of the study declare that they have no conflicts of interest.