Researchers from the University of Missouri School of Medicine have discovered how obstructive sleep apnea (OSA) changes the profiles of immune cells in the blood, leading to a unique cellular signature that can accurately detect obstructive sleep apnea in children.
OSA affects 22 million people in the U.S. including children. More than 10% of all children habitually snore, a hallmark symptom of potential OSA, but only one of every four to five snoring children actually suffers from sleep apnea. OSA in children is linked to a higher risk of cognitive, behavioral, metabolic and cardiovascular complications in children. The gold standard for diagnosis is a sleep study called Polysomnography (PSG), which monitors brain waves, blood oxygen levels, heart rate, breathing, eye and leg movements. But researchers have found a blood test may also offer a precise method to diagnose OSA.

“Our research has found that OSA induces changes to the diversity of the immune cells in the body that protect us against harmful viruses, bacteria and diseases,” said Rene Cortese, PhD, former assistant professor in the Department of Child Health and the Department of Obstetrics, Gynecology and Women’s Health. “These changes result in a unique gene signature that can be used to diagnose OSA with extremely high precision.”
Cortese’s team collected cellular samples from 11 children who were diagnosed with OSA through PSG, and 11 other asymptomatic healthy children without OSA. Using a process called single cell transcriptional profiling combined with traditional gene expression analysis, the team discovered the OSA patients exhibited a decline in the percentage of T-helper immune cells. Those patients also showed elevated levels of cMonocyte cells, a type of white blood cell, and a higher number of atypical B-cells, the producers of antibodies that fight bacteria and viruses.
“Based on these findings, we identified a molecular signature consisting of 32 genes, which distinguished children with OSA from children without sleep apnea with high precision,” Cortese said. “We then tested this signature array in a different and much larger group of non-snoring and snoring children where the gene expression was assessed using a less complex technology. Yet, the signature was able to identify with more than 95% accuracy in which children OSA was present.”
“This is a promising discovery that will require future validation to assess the performance of this gene signature and to confirm the utility of this signature in the clinic,” Cortese said.
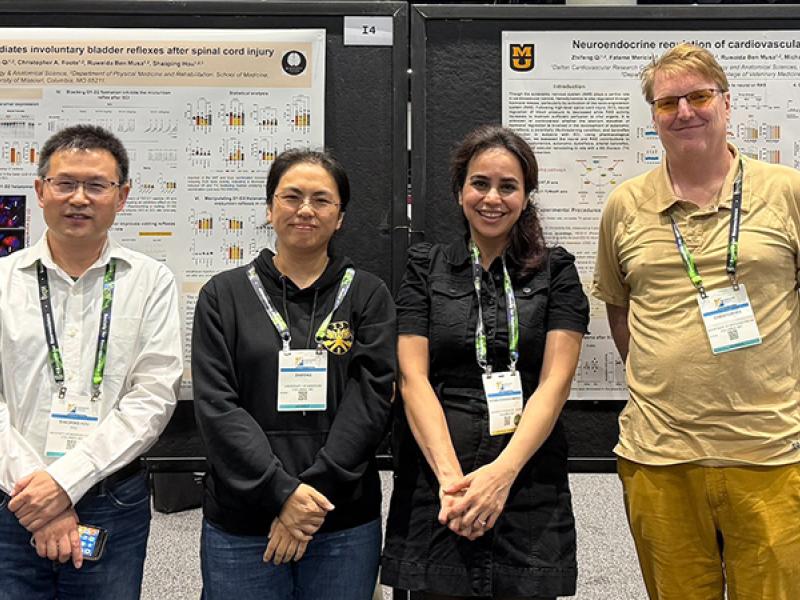
In addition to Cortese, the study authors include MU colleagues Leila Kheirandish-Gozal, MD, former director of the Child Health Research Institute; David Gozal, MD, the former Marie M. and Harry L. Smith Endowed Chair of Child Health; Kylie Cataldo, research specialist; and Justin Hummel, Institute for Data Science and Informatics.
Their study, “Single-cell RNAseq uncovers cellular heterogeneity and provides a signature for pediatric sleep apnea,” was recently published in the European Respiratory Journal.
This work was partially supported by grants from the BioNexus KC Patton Trust Research Grant, Tier 2 and TRIUMPH grants from the University of Missouri, and a Leda J. Sears Charitable Trust grant. The authors disclose no conflicts of interest.