The National Institutes of Health (NIH) has awarded a team of researchers, which includes a pair from the University of Missouri School of Medicine, a grant worth $3.2 million to test a treatment for Type 1 diabetes that does not require several insulin injections each day.
Pancreatic islet transplantation is an experimental treatment for Type 1 diabetes in which surgeons transplant clusters of pancreas cells from a deceased donor into a vein that carries blood to the liver of a person with Type 1 diabetes. The cell clusters then make and release insulin in the recipient’s body, potentially preventing the need for regular insulin injections. A major limitation of islet transplantation is the scarcity of donors and the need for lifelong use of immunosuppressive drugs to control rejection.
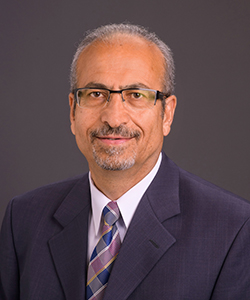
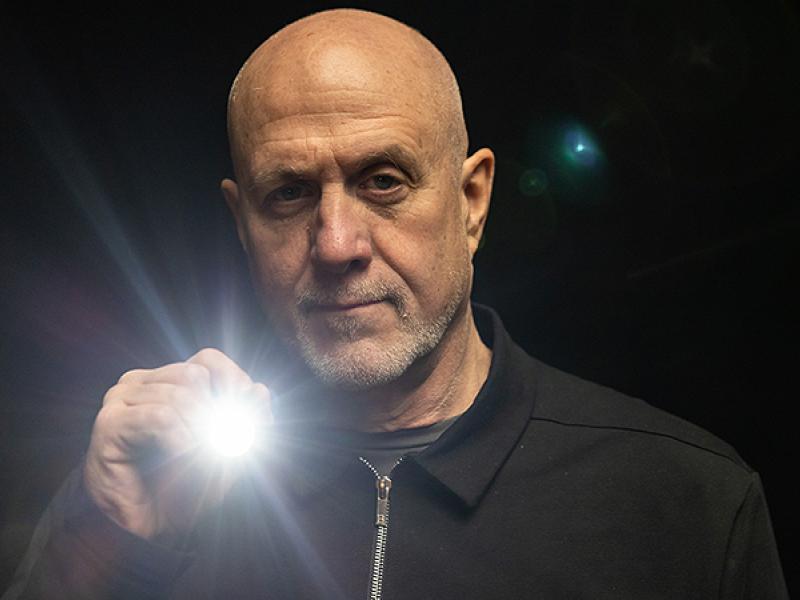
MU School of Medicine researchers Haval Shirwan, PhD, and Esma Yolcu, PhD, both professors of Child Health and Molecular Microbiology and Immunology, are part of a grant that involves researchers from the Georgia Institute of Technology, Harvard University/Massachusetts General Hospital, and Washington University in St. Louis to study a novel approach where a type of self-renewing stem cell is converted into an insulin-producing beta cell, then clusters of those cells are transplanted from a test tube into patients with Type 1 diabetes. To protect the stem cells from rejection, the transplant will include a microgel mixture that contains a protein designed to kill immune cells that identify the transplanted cells as a foreign threat.

“There is an unlimited source of stem cells, which solves the bottleneck currently associated with donor cells,” Shirwan said. “To ensure these cells are not destroyed after transplantation, we have developed a protein that will be included in the microgel mixture that will protect the transplanted cells by eliminating graft destroying immune cells, while expanding those beneficial to the survival of the graft. If successful, this approach will eliminate the need for life-long use of immunosuppression and be a game changer for the treatment of Type 1 diabetes.”
The stem cell to beta cell conversion transplant will initially be tested on preclinical models. If successful, it would eventually be tested on humans, with the potential to benefit those suffering from similar chronic diseases.
“This highly significant and innovative strategy is fundamentally different from ongoing work in this field,” Yolcu said. “If successful, this technology could benefit other transplant patients who require lifelong immunosuppression. The potential of this research is wide reaching and very exciting.”
This grant is an example of bench-to-bedside research, or how laboratory results are directly incorporated into use by patients in order to help treat different diseases and disorders, a hallmark of MU’s most ambitious research initiative, the NextGen Precision Health initiative.
Highlighting the promise of personalized health care and the impact of large-scale interdisciplinary collaboration, the NextGen Precision Health initiative is bringing together innovators like Shirwan and Yolcu from across MU and the UM System’s three other research universities in pursuit of life-changing precision health advancements. It’s a collaborative effort to leverage the research strengths of MU toward a better future for the health of Missourians and beyond. The Roy Blunt NextGen Precision Health building at MU anchors the overall initiative and expands collaboration between researchers, clinicians and industry partners in the state-of-the-art research facility.