Two University of Missouri School of Medicine researchers will receive $2.2 million of a $3 million grant from the U.S. Department of Defense to test a potentially life-changing, novel treatment for millions of people with Type 1 diabetes. The treatment is designed to stop the immune system from rejecting insulin-producing cell clusters transplanted from another person’s pancreas.
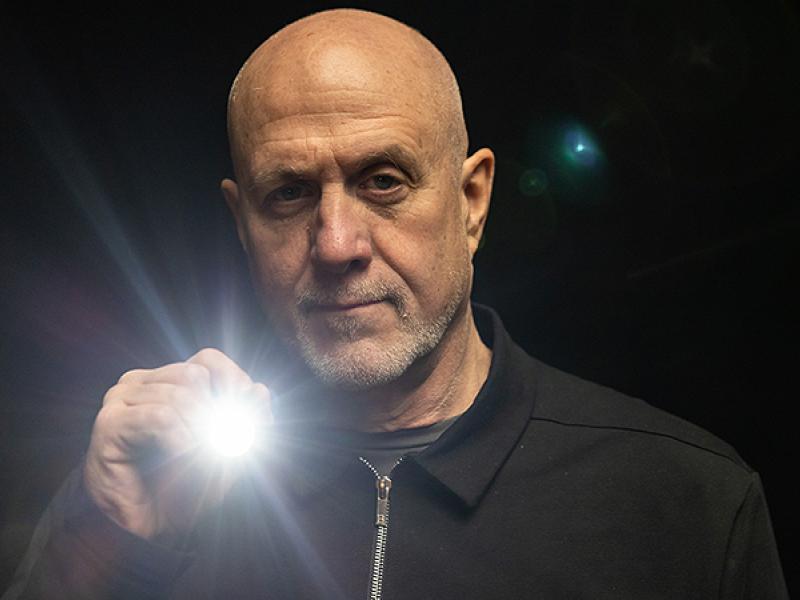
“Diabetes is one of the leading causes of death among military personnel, veterans, and the general public with an estimated annual cost of $242 billion,” said grant co-recipient Haval Shirwan, PhD, professor of child health and molecular microbiology and immunology. “Type 1 diabetes is an autoimmune disease where insulin producing cells are mistakenly attacked by the immune system and destroyed. Type 1 diabetes affects 1.6 million people in the U.S. with annual health care cost exceeding $16 billion.”
Pancreatic islet transplantation is a treatment for Type 1 diabetes in which surgeons transplant clusters of pancreas cells from a deceased donor into a vein that carries blood to the liver. The cell clusters then make and release insulin in the recipient’s body, potentially preventing the need for regular insulin injections. A major current limitation of islet transplantation is the need for lifelong use of immunosuppressive drugs to control rejection. These drugs are not always effective in controlling rejection and also have significant adverse effects on the recipient.
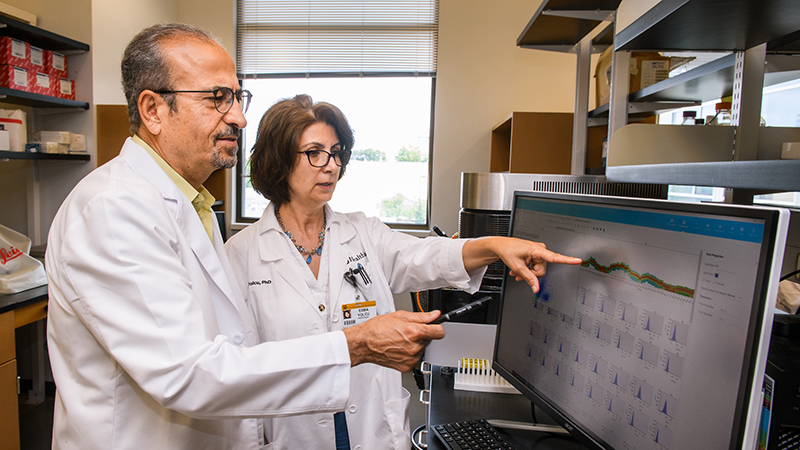
“Two distinct and opposing immune mechanisms regulate rejection of transplanted pancreatic cell clusters,” said grant co-recipient Esma Yolcu, PhD, professor of child health and molecular microbiology and immunology. “Destructive T effector (Teff) cells kill the transplanted clusters, while T regulatory (Treg) cells control the Teff cells and shield the transplanted clusters from rejection. Previous approaches have targeted Teff or Treg cells separately. We will target both simultaneously.”
Shirwan and Yolcu will work with Cornell University researchers, who received $922,000, to test a novel approach that uses a liquid droplet containing two biologics — drugs that contain components of living organisms — for targeted delivery to and controlled release within the transplanted pancreas cell cluster. These two biologics are designed to kill the Teff cells while expanding protective Treg cells, tilting the balance towards acceptance of the transplanted cell clusters, thus avoiding the use of chronic immunosuppression. The tests will initially involve mice, but the researchers hope to eventually progress to human trials.
“This is an exciting collaboration with our colleagues at Cornell to move a concept we developed for Type 1 diabetes from bench to bedside,” Shirwan said. “The long-term vision of this technology lies in its scope and scalability to broader populations beyond islet transplants, including all transplant types and other autoimmune diseases.”
The Department of Defense grant will begin in August and run through 2025.
Shirwan and Yolcu are among the first researchers who will move into the NextGen Precision Health building at the University of Missouri when it opens in October 2021. This initiative will expand collaboration in personalized health care and the translation of interdisciplinary research for the benefit of society. The NextGen Precision Health building at Mizzou anchors this statewide initiative, which aims to unite government and industry leaders with innovators from across the system’s four research universities in pursuit of life-changing precision health advancements. The University of Missouri System’s bold NextGen initiative highlights the promise of personalized health care and the impact of large-scale interdisciplinary collaboration.

Highlighting the promise of personalized health care and the impact of large-scale interdisciplinary collaboration, the NextGen Precision Health initiative is bringing together innovators from across the University of Missouri and the UM System’s three other research universities in pursuit of life-changing precision health advancements. It’s a collaborative effort to leverage the research strengths of Mizzou toward a better future for the health of Missourians and beyond. The Roy Blunt NextGen Precision Health building at MU anchors the overall initiative and expands collaboration between researchers, clinicians and industry partners in the state-of-the-art research facility.