A University of Missouri study on clinical outcomes after biologic knee restoration surgery found patients who received cartilage grafts that were stored using a novel graft preservation system had better outcomes than those who received grafts preserved by traditional methods.
The study compared the results of patients who received osteochondral allograft transplants at MU Health Care’s Missouri Orthopaedic Institute. The patients who received grafts that were stored in the Missouri Osteochondral Preservation System (MOPS℠) had an initial success rate of 84% compared to 60% for those who received grafts that were stored by traditional methods.
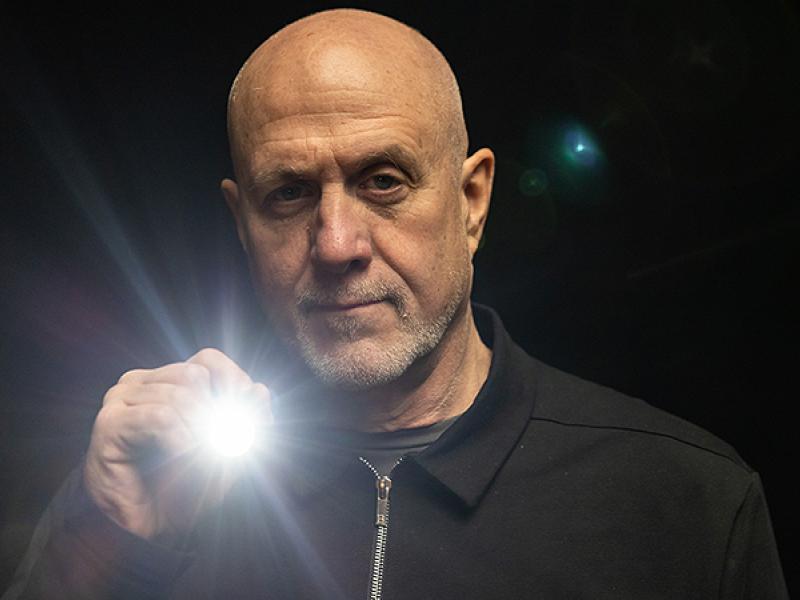
“The initial evidence from this large prospective clinical study suggests that the combination of MOPS℠ preservation and precision-medicine techniques for graft cutting and implantation, together with patient-specific rehabilitation protocols, patient education and counseling, can result in significantly better initial outcomes compared to what has been done in the previous 40 years,” said study co-author James Stannard, MD, Hansjörg Wyss Distinguished Chair of Orthopaedic Surgery and medical director of the Missouri Orthopaedic Institute.
James Cook, DVM, PhD, OTSC, director of the Orthopaedic Research Division at MU, led a team of scientists who developed MOPS, a system designed at MU using a novel cartilage-preserving solution and specially designed storage conditions that allow osteochondral allografts to be stored for twice as long as traditional storage methods and still maintain necessary cell viability levels. Surgeons at the Missouri Orthopaedic Institute have performed osteochondral allograft transplants using grafts stored in MOPS℠ since 2016 and now use those grafts exclusively based on multiple peer-reviewed scientific studies.
“MOPS℠ was developed at the University of Missouri School of Medicine’s Thompson Laboratory for Regenerative Orthopaedics in collaboration with scientists at Columbia University in New York and has proven to be a big step forward in improving outcomes for patients,” Cook said. “It has been really rewarding to work with a team of people who are passionate about improving orthopaedic healthcare, and to see all of our hard work come through to benefit the patients we were thinking about from day one. The other really special part is that this technology helps to decrease associated healthcare costs, better honor the precious gifts of donated tissue from organ donors and show gratitude to donor families.”
The current study looked at 194 patients who were one to four years removed from their osteochondral allograft procedure. Of those patients, 137 received MOPS℠ grafts and 57 received grafts preserved by traditional methods. The initial success rate, as defined by a surgery that did not fail or require a revision throughout the study period, was 24% better for patients who received a MOPS℠ graft.
In addition to reviewing the preservation method, the study also looked at specific postoperative rehabilitation protocols to recover from cartilage transplant procedures in the knee. Those patients that did not comply with the prescribed rehabilitation during the first year after surgery were 6.7 times more likely to be associated with non-successful outcomes than those who followed the prescribed protocol.
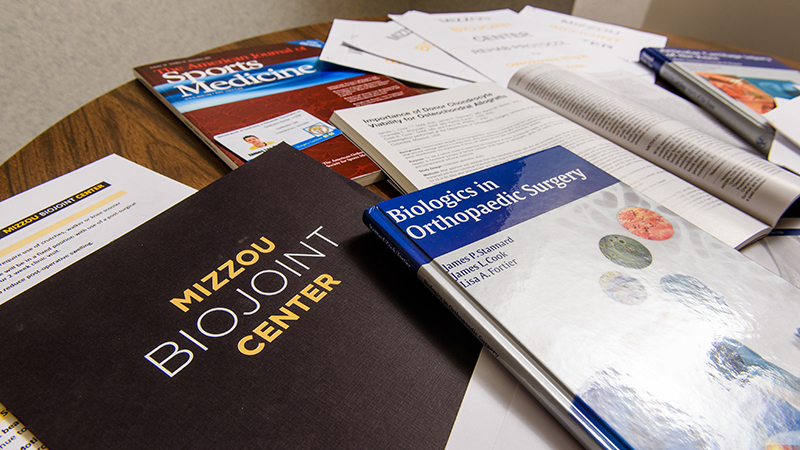
Written by James Stannard, MD, and James Cook, DVM, PhD, OTSC, the study, “Prospective Assessment of Outcomes after Primary Unipolar, Multisurface, and Bipolar Osteochondral Allograft Transplantations in the Knee: A Comparison of 2 Preservation Methods” was recently published in the American Journal of Sports Medicine.